Invasive Ductal Carcinoma (IDC)
Invasive ductal carcinoma key highlights
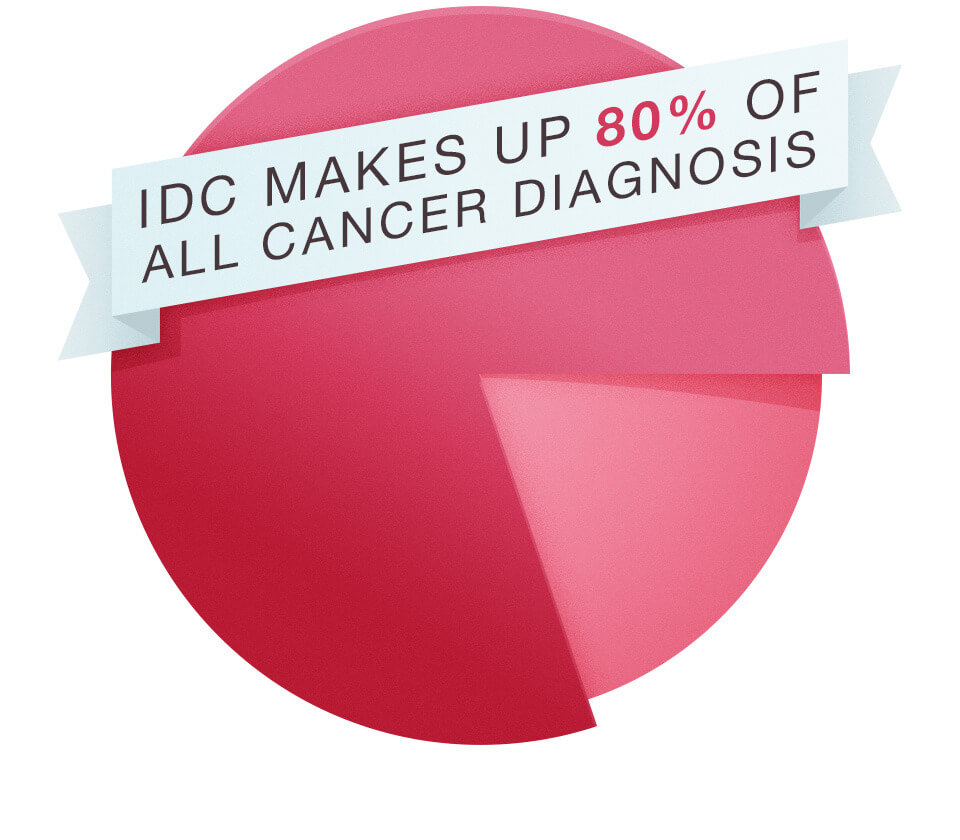
- Invasive ductal carcinoma (IDC) is the most common type of breast cancer, making up 80% of all breast cancer diagnoses.
- IDC is the most common type of breast cancer in men.
- IDC is also called infiltrative ductal carcinoma.
- There are many treatment options available for IDC.
Jump to
What is invasive ductal carcinoma (IDC)?
What is the difference between IDC and DCIS?
How serious is IDC?
Signs and symptoms of IDC
Causes and risk factors of IDC
IDC diagnosis
IDC stages
IDC grades
Prognostic factors of IDC
Treatment of IDC
IDC prognosis and survival rate
Resources and support for IDC
Invasive ductal carcinoma FAQs
IDC stories of hope
What is invasive ductal carcinoma (IDC)?
Invasive ductal carcinoma (IDC) occurs when cancer cells that began forming in a milk duct of the breast spread beyond the duct into other breast tissue or to other areas of the body. The term “invasive” refers to the way the cancerous cells spread to (or invade) the surrounding breast tissue or other body parts.
There are several types of invasive ductal carcinoma. The most common types of IDC include:
- HER2-positive (HER2+) breast cancer: Occurs when there is too much human epidermal growth factor 2 (HER2) in the body, causing cancer to grow and spread quickly
- ER-positive (ER+) breast cancer: Cancerous cells receive signals from the hormone estrogen, causing them to grow
- PR-positive (PR+) breast cancer: Cancerous cells receive signals from the hormone progesterone, causing them to grow
- Triple-positive breast cancer: An aggressive form of breast cancer in which all three receptors test positive: ER+, PR+, and HER2+
- Triple-negative breast cancer: An aggressive form of breast cancer in which all three receptors test negative: ER-, PR-, and HER2-
There are multiple treatment options available for IDC. Cancer staging done by a physician, along with a physical exam and patient medical history, can help identify the best treatment options.
What is the difference between invasive ductal carcinoma (IDC) and ductal carcinoma in situ (DCIS)?
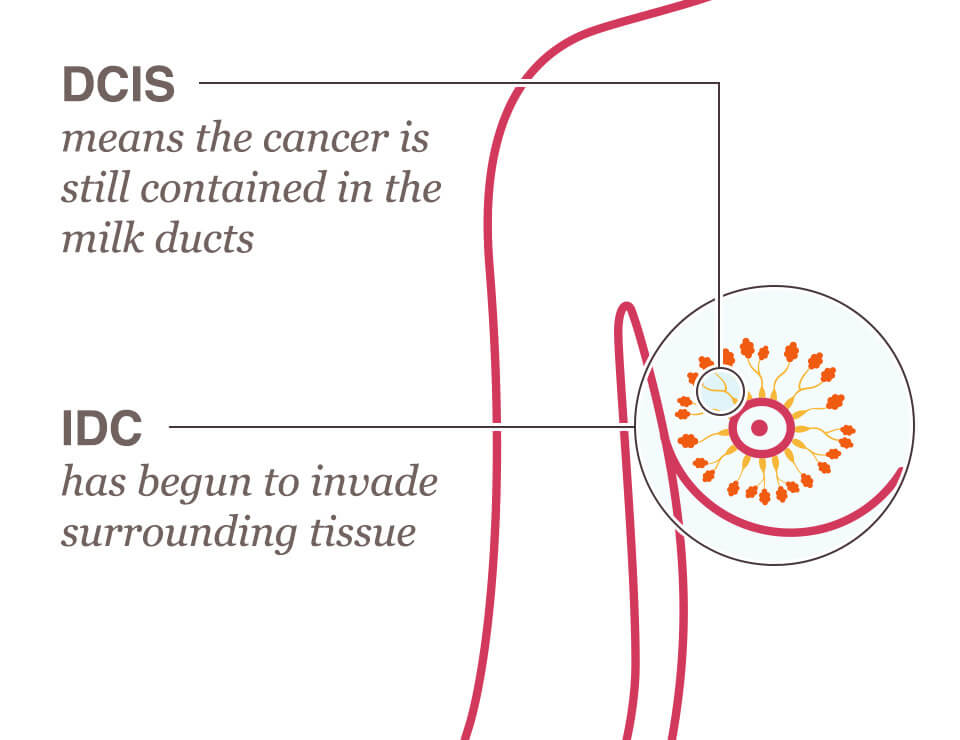
Ductal carcinoma in situ (DCIS) is non-invasive breast cancer; it forms and remains contained within the milk duct and has not yet spread to any other area of the breast or elsewhere in the body. In invasive ductal carcinoma (IDC), the cancer is invasive; it forms in the milk duct and begins spreading, invading the surrounding breast tissue. If left undetected and untreated, IDC can metastasize (spread) to other areas of the body, starting by invading the lymph nodes or bloodstream.
How serious is invasive ductal carcinoma?
The severity of IDC depends on the stage at diagnosis, how far the cancer has spread, and its prognostic factors (ER, PR and HER2 receptors). When caught and treated in an early stage, the survival rate for IDC is very good. Survival rates for IDC decline the more progressed the cancer is when detected and treated.
Without prompt diagnosis and treatment, IDC can spread to lymph nodes and throughout the body, traveling through the bloodstream. Mammograms and other screenings are vital for the early detection of IDC, before it has a chance to spread and when it is most treatable.
Invasive ductal carcinoma signs & symptoms
Not all IDC has detectable signs and symptoms, especially when it is in the early stages. If signs and symptoms are present, they may be similar to those of other types of breast cancer.
If present, invasive ductal carcinoma (IDC) signs and symptoms may look like:
- A new lump or thickening in or near the breast or in the underarm area
- Any unexplained change in the size or shape of the breast, including swelling or shrinkage (especially if on one side only)
- Dimpling anywhere on the breast
- Puckering in the skin of the breast
- A nipple turned inward (inverted) into the breast
- Discharge (fluid) from the nipple (particularly clear or bloody discharge)
- A change in the skin texture, discoloration, swelling, or an enlargement of pores in the skin of the breast (some describe this as similar to an orange peel’s texture)
- Scaly, red, or swollen skin on the breast, nipple, or areola
- Recent asymmetry (unequal or lack of sameness) of the breasts
It is important to remember that not all breast lumps or other breast changes are breast cancer. In fact, the majority of breast lumps are not cancerous. However, all breast changes, including new lumps or skin changes, should be reported to your doctor promptly.
Invasive ductal carcinoma cause and risk factors
The exact cause of invasive ductal carcinoma is not known or fully understood. While the underlying cause of IDC remains unknown, it results in a breast milk duct undergoing a genetic change (mutation) that causes the mutated cells to grow and divide rapidly. This accumulation of mutated cells can then form a cancerous tumor or mass, which is invasive ductal carcinoma.
Though the cause is unknown, there are certain risk factors for IDC that researchers have identified. Risk factors for IDC can be both genetic and lifestyle & environmental.
Genetic risk factors for invasive ductal carcinoma
Genetic risk factors are inherited or passed down from parent to child through the genes. These factors are out of a person’s control and cannot be changed.
Genetic risk factors for invasive ductal carcinoma may include:
- Gender: Though men can develop IDC, it is nearly 100 times more common in women than in men.
- Age: The majority of women diagnosed with IDC are 55 years old or older, though it can happen at any age.
- Race: Black women are more likely than white women to be diagnosed with aggressive forms of invasive ductal carcinoma, such as triple-negative breast cancer, and Black women are often diagnosed at a younger age and experience a higher mortality rate than white women.
- Family and personal medical history: Women with a first-degree relative with breast or ovarian cancer have a higher risk of developing breast cancer; a past personal history of breast cancer also increases a woman’s risk of cancer recurring or coming back.
- Dense breast tissue: Dense breast tissue makes lumps or other abnormalities harder to detect, increasing the risk of breast cancer. Beginning in September 2024, breast imaging radiologists are required to include how dense the breast tissue is in the mammogram report. Density looks white on a mammogram and breast cancer in the form of IDC is also white, making it hard to differentiate healthy dense breast tissue from IDC cells. If the density of the breast tissue is high, additional imaging, such as an ultrasound or MRI, may be warranted.
- Genetic mutations: A mutation (or change) in a BRCA gene (BRCA1 or BRCA2) or other breast cancer gene increases a woman’s risk of developing breast cancer.
Lifestyle & environmental risk factors for invasive ductal carcinoma
Lifestyle & environmental risk factors are avoidable risk factors that are often under a person’s control, meaning they can be managed and reduced.
Lifestyle & environmental risk factors for invasive ductal carcinoma may include:
- Lack of physical activity
- Poor diet
- Being overweight or obese
- Drinking alcohol or smoking
- Long-term use (6 months or more) of hormonal replacement therapy (HRT)
Invasive ductal carcinoma (IDC) diagnosis
Invasive ductal carcinoma is usually diagnosed through a combination of different tests and imaging. Many cases of IDC are first detected on an annual screening mammogram. All women age 40 and over should receive an annual screening mammogram to check for breast cancer in the early stages, when it is easiest to treat.
If there is a significant family history of breast cancer or a known genetic mutation, breast imaging in some form may begin earlier than age 40. This should be discussed with your doctor.
If a screening mammogram comes back with abnormal results, or if breast cancer signs and symptoms are present, the following diagnostic tests may then be performed:
- Diagnostic mammogram: A diagnostic mammogram is a more detailed, in-depth x-ray of the breast than a screening mammogram.
- Breast ultrasound: A breast ultrasound is an image of the breast formed by sound waves and can offer more details than a mammogram.
- Breast MRI: A breast MRI uses magnetic waves and radio energy to provide a detailed picture of the inside of the breast.
- Breast biopsy: A breast biopsy removes a small portion of suspicious tissue or fluid from the breast using a needle. The sample is then studied under a microscope to determine if cancerous cells are present.
Invasive ductal carcinoma stages
When breast cancer has been identified and diagnosed, it will be given a breast cancer stage. The stage of breast cancer indicates whether the cancer has spread within the breast or elsewhere in the body.
Like other types of invasive breast cancer, invasive ductal carcinoma will be assigned a stage between 1 and 4. Generally, the lower the stage, the less progressed the cancer.
Invasive ductal carcinoma stages are as follows:
IDC Stage | Indication |
|---|---|
Stage 1 invasive ductal carcinoma | Stage 1 IDC means the cancer has spread from the milk duct into the breast tissue but hasn’t spread to the lymph nodes or elsewhere. |
Stage 2 invasive ductal carcinoma | There are two substages in Stage 2 IDC: Stage 2A: The cancerous tumor is large, between 2-5 centimeters, but has not spread. Stage 2B: The cancerous tumor is smaller than 2 centimeters but has spread to nearby lymph nodes. |
Stage 3 invasive ductal carcinoma | There are three substages in Stage 3 IDC: Stage 3A: The cancer has spread to nearby lymph nodes. Stage 3B: The cancer has invaded the chest wall or breast skin, such as in inflammatory breast cancer. Stage 3C: The cancer has spread to lymph nodes near the collarbone. |
Stage 4 invasive ductal carcinoma | Stage 4 IDC means that the cancer has spread to distant areas of the body, such as the bones, liver, lungs, or brain. This is also called metastatic breast cancer. |
Invasive ductal carcinoma grades
When breast cancer is diagnosed, it will be given a grade. A cancer grade is a numbering system that describes how abnormal the cancerous cells look under a microscope. Cancer grades are not to be confused with cancer stages; they are separate and different.
All breast cancer is graded between 1 and 3. Generally, the lower the grade, the less aggressive the cancer.
Invasive ductal carcinoma grades are as follows:
IDC Grade | Indication |
|---|---|
Grade 1 | The cancerous cells look much like normal breast cells and tend to grow slowly. |
Grade 2 | The cancerous cells look much like normal breast cells and tend to grow at a moderate pace (faster than Grade 1). |
Grade 3 | The cancerous cells look distinctly different from normal breast cells and tend to grow quickly. Grade 3 IDC presents an increased chance of breast cancer recurrence in the future. |
Prognostic factors of invasive ductal carcinoma
Prognostic factors are the characteristics of specific cancers. After a biopsy, a pathologist will create a pathology report outlining the prognostic factors of the breast cancer, which will be used to determine the best treatment options.
There are 3 specific prognostic factors pathologists look for to help determine IDC treatment:
- Estrogen receptor status: The cancer is called estrogen receptor-positive (ER+) if estrogen receptors are found in the cancerous cells. This means that estrogen stimulates these specific IDC cells to grow and multiply. The higher the percentage or ER+ cells, the more favorable this prognostic factor is. When the cells are ER+, hormonal therapy will be recommended as a key part of treatment for prevention of recurrence.
- Progesterone receptor status: The progesterone receptor is also determined and, if positive (PR+), is also a favorable prognostic factor.
- HER2 receptor status: HER2, or human epidermal growth factor receptor 2, helps determine if the IDC cells are aggressive and overproducing the HER2 protein.
Treatment of invasive ductal carcinoma (IDC)
There are many treatment options available for invasive ductal carcinoma. The best treatment plan for an individual with IDC will depend on the type, stage, grade, and prognostic factors of the cancer, as well as the patient’s personal medical history. There are several types of treatment for invasive ductal carcinoma.
Breast surgery
Breast surgery is often performed to surgically treat IDC. There are different types of breast cancer surgery.
Lumpectomy
A lumpectomyis breast-conserving surgery that removes only the cancerous tumor and a small margin of healthy tissue surrounding it. A lumpectomy is sometimes called a partial mastectomy and is usually used to treat only early-stage IDC when the cancerous tumor is small. A sentinel node biopsy will also be performed to determine if the IDC has spread beyond the breast itself. The pathologist will also look for the presence of lymphatic invasion (cancerous cells in the lymph nodes) and/or vascular invasion (cancerous cells in the bloodstream) within the breast tumor itself, which, when found, increases the risk of the breast cancer having spread elsewhere in the body.
A lumpectomy may be followed by radiation to ensure that all cancerous cells have been destroyed. If chemotherapy is administered before surgery to shrink the tumor (neoadjuvant chemotherapy), the option of performing a lumpectomy instead of a mastectomy may be possible.
Mastectomy
A mastectomy is the surgical removal of the breast and is usually used to treat patients with multiple cancerous tumors, aggressive or later-stage IDC, or those with large invasive tumors. There are several different types of mastectomies, including total simple mastectomy, skin-sparing mastectomy, and modified radical mastectomy. A sentinel node biopsy will likely be performed at the time of a mastectomy to determine if the cancer has spread. A mastectomy may be performed with or without breast reconstruction.
Breast Cancer Surgery eBook
Be prepared for your surgical oncology appointments by learning about the different types of breast cancer surgeries with the free Breast Cancer Surgery eBook.
Download the free eBookRadiation
Radiation uses high-energy rays to destroy cancer cells and may be used after lumpectomy surgery to treat IDC and reduce the chance of the cancer coming back. It is not usually used after a mastectomy unless the tumor was large or positive lymph nodes were found. Radiation is sometimes used to treat bone pain associated with Stage 4 metastatic breast cancer.
Chemotherapy
Chemotherapy uses a combination of drugs to destroy cancer cells or slow their growth. The use of chemotherapy will depend on the prognostic factors—or features—of the breast cancer, such as ER, PR, and HER2 status. Other factors influencing the decision to use chemotherapy to treat invasive ductal carcinoma include the cancer stage, grade, tumor size, and whether the cancer has spread.
Chemotherapy may be given before surgery (neoadjuvant therapy) to reduce the tumor size, after surgery (adjuvant therapy) to reduce the chance of cancer returning, or both. The patient’s care team will help determine if, when, and what type of chemotherapy to administer to treat IDC.
Hormonal therapy
Hormonal therapy uses drugs to block or lower the levels of hormones, such as estrogen and progesterone, in the body, which can help slow or stop the growth of some breast cancers, including certain types of invasive ductal carcinoma. It may be given to women with hormone receptor-positive (ER+, PR+, ER/PR+) IDC before or after breast surgery, or it may be given to certain Stage 4 IDC patients to help manage symptoms. Additionally, CDK4/6 inhibitors with hormonal therapy are being used for Stage 4 breast cancer and Stage 3C breast cancer when the breast cancer is ER+ and HER2-.
Common hormonal therapy drugs include tamoxifen for premenopausal women and aromatase inhibitors for postmenopausal women. Hormonal therapy is not used to treat triple-negative breast cancer (TNBC) since TNBC cells lack ER and PR hormone receptors.
Targeted therapy
Targeted therapy to treat invasive ductal carcinoma uses drugs that are directed (targeted) at the proteins in cancerous cells, most commonly HER2 proteins, slowing down or stopping cell growth. Unlike chemotherapy, targeted therapy is directed at specific types of cancerous cells rather than all cells—whether healthy or not—as in chemotherapy.
Immunotherapy
Immunotherapy is a type of targeted therapy that may be used to treat Stage 4 metastatic breast cancer. Immunotherapy uses the patient’s immune system to fight the cancer.
Treatment for invasive ductal carcinoma is not a one-size-fits-all approach. Instead, your oncologist and care team will be able to recommend the treatment—or combination of treatments—that will be best for you.
Invasive ductal carcinoma prognosis and survival rate
When diagnosed and treated in the localized stage, before the cancer has a chance to spread, the prognosis for invasive ductal carcinoma is very good. According to the American Cancer Society, the 5-year relative survival rate for localized invasive ductal carcinoma is over 99%. If the cancer has spread into nearby tissue or has metastasized into other areas of the body, the 5-year survival rate begins to decrease.
Survival rates for invasive ductal carcinoma are grouped into three stages: localized, regional, and distant. Each stage has its own 5-year relative survival rate. Keep in mind that statistics such as this are only tracked for 5 years, which is why the statistic is measured in a 5-year increment. This means that many patients, especially those with early-stage breast cancer, live long and healthy lives.
5-year relative survival rates for invasive ductal carcinoma
| SEER* Stage | 5-year relative survival rate |
| Localized: There is no sign that cancer has spread outside of the breast. Includes only invasive breast cancer, not DCIS. | >99% |
| Regional: The cancer has spread outside of the breast to nearby structures or lymph nodes. | 87% |
| Distant: The cancer has spread to different parts of the body, such as the bones, liver, lungs, or brain. | 33% |
| All SEER stages combined | 92% |
**Table information provided by the American Cancer Society
Invasive ductal carcinoma recurrence
Invasive ductal carcinoma recurrence is when the cancer comes back, either months or years later, after initial successful treatment. Recurrence can be local, with cancer reappearing at or near the original site of the breast cancer, regional, involving the lymph nodes under the arm of in the area of the clavicle, or distant, with breast cancer cells appearing in other areas of the body, most commonly in the bones, liver, lungs, or brain.
It’s important to keep in mind that every individual and every cancer is unique. There is no statistic that can accurately predict the chances of a breast cancer recurrence. IDC recurrence rates vary widely and are based on several factors, including the type and stage of the original cancer, the treatments undertaken, and the length of time since the completion of the original treatment.
Though IDC recurrence cannot be fully prevented, there are several ways to lower the risk of recurrence, including:
- Staying in contact with your oncologist for follow-up appointments
- Taking hormonal therapy exactly as prescribed (if cancer was hormone receptor-positive)
- Continuing early detection (mammograms and breast self-exams) on any remaining breast tissue, as recommended by your doctor
- Eating well to ensure proper nutrition
- Maintaining a healthy weight
- Participating in regular physical activity or exercise
- Not smoking or drinking alcohol
Resources and support for invasive ductal carcinoma
Support is necessary for those living with invasive ductal carcinoma and survivors. Many organizations offer support groups for patients and survivors to share their experiences, ask questions, and form relationships with individuals going through similar circumstances.
NBCF Patient & Survivor Support Group
NBCF offers free in-person and virtual support groups for women nationwide. Learn more about and join an NBCF support group.
NBCF Support GroupOther organizations offer support groups as well, including groups for specific needs, such as for young adults with breast cancer or those facing Stage 4 metastatic breast cancer. Click here to look for a support group that fits your needs and situation.
Invasive ductal carcinoma (IDC) FAQs
Is invasive breast cancer aggressive?
Invasive breast cancer, such as invasive ductal carcinoma, tends to be more aggressive than non-invasive breast cancer (ductal carcinoma in situ, DCIS). However, the level of aggressiveness depends on the type, stage, prognostic factors, and grade of invasive breast cancer.
Generally, triple-negative breast cancer and inflammatory breast cancer tend to be the most aggressive types of invasive breast cancer because they are faster growing and harder to treat than some other types. Grade 3 breast cancer also tends to be more aggressive than other grades.
Is invasive ductal carcinoma curable?
Many healthcare professionals no longer use the word “cured” when referring to the end of breast cancer treatment. Instead, they will often refer to the patient as “cancer-free.” With vigilant treatment and support, many individuals diagnosed with Stage 1-3 invasive ductal carcinoma are declared cancer-free at the end of treatment.
How long can you live with invasive ductal carcinoma?
The length of time a person can live with invasive ductal carcinoma depends on the type and stage of the cancer at diagnosis. When detected and treated early, the prognosis and life expectancy for those with IDC is very good, and many may expect to live an equally long life as someone who never experienced invasive ductal carcinoma.
Is invasive ductal carcinoma hereditary?
Invasive ductal carcinoma and other types of breast cancer may be hereditary (or genetic) in 5-10% of cases. While the type of breast cancer passed through the genes is not hereditary, it is statistically more likely to be IDC since it is the most common form of breast cancer. This means that in 5-10% of breast cancer cases, a breast cancer gene mutation was passed down from a parent to a child. Individuals with an inherited BRCA gene mutation or other breast cancer gene mutation have a 45-65% chance of developing breast cancer in their lifetime.
Can invasive ductal carcinoma spread?
Yes. IDC is called “invasive” breast cancer because it can spread—or invade—healthy breast tissue, lymph nodes, or into other organs of the body, increasing the stage of IDC. Invasive ductal carcinoma is most treatable when it is caught and treated early before it has a chance to spread.
Does invasive ductal carcinoma return?
Even after successful treatment, IDC can return in the form of a breast cancer recurrence. There are different types of recurrence. A local recurrence is when cancer returns at or near the original location in the breast; a regional recurrence is when cancer returns in the lymph nodes near the original site of the cancer; and a distant recurrence is when breast cancer cells reappear in distant areas of the body, such as the bones, liver, lungs, or brain. A distant recurrence of invasive ductal carcinoma is called metastatic breast cancer.
Invasive ductal carcinoma stories of hope
No matter the type of breast cancer, NBCF is here to offer help and hope. Read invasive ductal carcinoma stories of hope on the NBCF blog:
Trisha’s Journey as a Young Mom with Breast Cancer
When Hair Loss is About More than Just Hair: Jessica’s Story
One Year Later: An Update on Gigi’s Survivorship
Sources:
Johns Hopkins Medicine
Cleveland Clinic
Penn Medicine
Moffitt Cancer Center
Penn Medicine



